A short video on how to dress your toes following nail surgery

A short video on how to dress your toes following nail surgery


So what is capsulitis?
Well simply speaking it is inflammation of the joint capsule. Ligaments around
joints and help form a capsule. Joint capsules help your joints to function properly the
ligaments hold them together. It is these that get inflamed. This can lead to toe dislocation
if it not treated appropriately. In fact, capsulitis is sometimes known as predislocation
syndrome. Capsulitis is a condition that can manifest in people of any age.
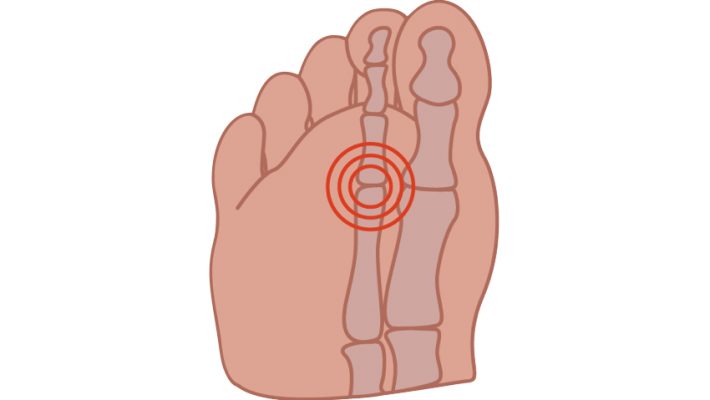
Although any joint in the foot can be subject to capsulatus the 2nd toe joint, under the ball
of the foot is most frequently affected and the metatarsals in general are the joints most
frequently troubled by capsulitis.
Causes vary but increased pressure particularly if the 2nd toe is the longest will cause more
pressure on that metatarsal head. Other causes include large bunions which can also be
prone to capsulitis themselves or by putting more pressure on the adjacent second
metatarsal lead to problems there. An unstable arch of the foot and footwear which may
include high heels, narrow toe box or toe spring which is an elevated toe box common in
many shoes also predispose to this problem. Tight posterior muscle groups and tight or
unbalanced tendons in the foot may further exacerbate the situation. The problem is also
common in runners and sports men and women.
Symptoms, pain is always a feature and other symptoms may include redness, callous over
the area, increased space between toes, the feeling of walking on a stone and swelling
around the area.
Treatment is directed at the causes, and may include rest and reducing weight bearing
activities, padding, stretching. Insoles are often helpful to deflect the pressure/control the
foot.
Often a cutaway is used to reduce pressure under the area. Icing the area and laser is
very helpful to reduce the inflammation in combination with padding strapping and or
insoles or orthotics.

I have been seeing a lot of corns under the nail recently they are more common this time of year due to most people wearing closed in shoes. So I thought this month I would write about a few of the things podiatrists find under toenails.
Well undoubtedly the most common problem encountered under the nail are corns. Patients present with either pain in the middle of the nail or at the sides. Sometimes at the sides these corns are associated with ingrown or involuted nails where the nail is pushing onto the skin and that pressure creates a corn. If the nail has been treated but the toe is still sore often it is a corn that is too blame and even tiny corns here can cause a disproportionate amount of pain.
Corns under the middle of the nail are usually formed when the nail touches the top of the shoe, often they are difficult or even impossible to see and are only detected because of the pain. They can be removed painlessly and doing so gives great relief.
Haematoma or bruise under the nails are very common too, this can be caused by dropping something on the toe or similar acute trauma or by foot ware. I often encounter this in walkers and runners, particularly if going for long stretches down hill. The toe, usually the first or second gets squashed into the toe box of the shoe and the nail turns red/black.
Initially there can be inflammation of the skin around the nail and the whole toe is sore. The discolouration is blood and tissue fluid under the nail and if this is drained within the first few days there is immediate pain relief and sometimes the nail will not be lost. If left, the fluid eventually dries and hardens and as this is between the nail and the nail bed the nail will frequently come away. A new nail always grows but sometimes that nail is a little thicker than the original.
Fungus, which I have written about before is common under nails it can present as discolouration anything from white, yellow, green, brown or even black, often the nail becomes thick and may be crumbly and occasionally smelly. These do not usually present as a painful condition except of course if the fungus has made the nail very thick and it then interferes with foot ware.
There are many types of treatment available for nail fungus from topical paints and varnishes to laser and even tablets.
Skin cancer can be found under nails, Malignant Melanoma always has to be considered if there is discolouration without a history of trauma. These can even present like an ingrown toenail with swelling and inflammation. Here rapid referral for definitive diagnosis and excision are crucial.

Corns are painful lesions on the feet caused by mechanical stress to that particular area. This increased mechanical stress can be due to pressure from foot ware or changes in the foot or the way we walk.
There are several types of corns or Helomata which comes from Greek helos, meaning stone wedge. Hard corns, heloma dura usually occur underneath the foot or on the tops or ends of the toes and may even occur under the nails or in the sides of the nails. Soft corns or heloma molle only appear between the toes and are soft due to perspiration between the toes. Vascular and neurovascular, heloma vasculare and heloma neurovasculare tend to be long standing lesions where blood vessels and nerves have become involved. Finally seed corns or helomata miliare which are not really corns at all. They are not caused by increased stress or pressure on the skin but are simply plugs or beads of cholesterol often in non weight bearing areas.
Differential diagnosis, most commonly confused with verruca which are generally not painful on direct pressure which corns are. Veruca also always have a vascular and neurological element.
Complications, neglected corns are can be prone to infections particularly due to foots close confinement in a warm humid environment and the proximity to the ground. Ulceration may also occur where there is sever mechanical stress or due to loss of sensitivity as in the case of diabetic neuropathy.
Treatment is roughly divided into two parts removal of the corn, sharp debridement where the corn is removed by a podiatrist/chiropodist with a scalpel. This should be a painless procedure and give instant relief from the ongoing discomfort.
Occasionally the use of local anaesthetic is required in the case of neurovascular corns. Once the corn is out the aim of the treatment is to prevent it returning. Here eliminating the original causes is the priority, reducing the pressure from foot ware and mechanical stress.
This may be padding to the foot in the short term. Changing footwear, insoles, orthotics or silicone guards to redistribute pressure where there have been changes in the shape and function of the foot longer term to mitigate the underlying problems.
There are of course over the counter remedies, usually in the form of corn plasters and these come in two basic types.
Foam rings, these aim to reduce the pressure on the lesion. Medicated corn plasters which contain an acid (usually salicylic acid) which aims to soften and dissolve the corn. The danger here is that if great care is not taken medicated corn plasters and liquids can dissolve healthy skin. This may not only be painful but in the case of diabetics and those with poor circulation can also be very dangerous and should be avoided.
As usual my advice is if in doubt see a podiatrist who will be able to treat the presenting problem and also work towards a longer term resolution.
Philip Mann 686912307


The problem causes pain in the front central portion of the knee usually worse when running or walking up or down hill or going up and down stairs (down particularly). Often there can be pain when sitting with knees bent, which is why the condition is also known as theatre goers knee. Pain comes from behind the kneecap (Patella) where it contacts with the thigh bone (femur).
Prolonged excessive shearing forces between the back of the patella and the front of the femur as the patella no longer tracks nicely between the groves formed by the bottom of the femur.
The problem is usually caused by biomechanical dysfunction, over pull of the lateral quadriceps, excessive pronation or supnation (rolling in or rolling out) of the foot. Overuse in sports or activities which are tough on the knee can also lead to patella femoral syndrome, running, jumping, cycling often exacerbated by biomechanical problems.
This results in inflammation, pain and eventually thinning and softening (Chondromalacia) of the articular cartilage behind the patella and on the femur. The condition can also be secondary to fractures, Osteoarthritis and bony tumours, i.e. changes in the bony structure of the knee.
The problem is usually diagnosed on examination and history, although X-ray and MRI can be useful if the diagnosis is not straightforward.
Treatment can involve any or all of the following, controlling excessive biomechanical dysfunction (pronation or supination) of the feet and legs with either strapping or orthotics, quadriceps strengthening, stretching of posterior muscles of the leg and thigh, and sometimes direct treatment to the knee, laser, icing and anti-inflammatory drugs.
Treatment will depend on the severity and duration of the problem and identification of the underlying causes. Prognosis is full recovery, and a return to normal activities once underlying causes are identified and addressed. I think podiatrists are in a unique position the treat this problem as we are able to address the underlying biomechanical problems to resolve the condition. But then I am a bit biased!
Philip Mann Podiatrist/Chiropodist tel: 686 912 307 or www.footpodiatrist.com