Charcot foot is a condition associated with neuropathy (nerve damage) to the foot.
It can lead to deformity, ulceration and even amputation. Although this problem is associated with many conditions that involve neuropathy to the feet, these include nerve damage caused by toxins (ethanol, drug related), infection (leprosy), as well as spinal cord damage and a number of other diseases (Parkinson’s disease, HIV, sarcoidosis, rheumatoid arthritis and psoriasis).
But by far the most common underlying problem is Diabetes, in over 20 years of looking at feet I have only seen one patient with a Charcot foot who was not diabetic.
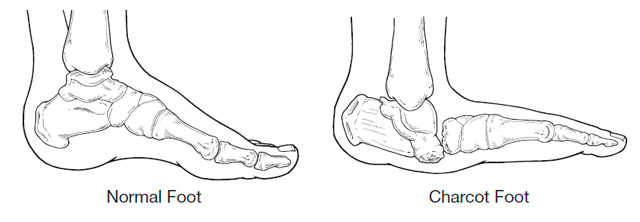
There is still some, shall we say discussion in the medical profession as to the exact disease process, but most agree that weakened bones in the foot exacerbated by loss of feeling and sometimes trauma start off an inflammatory process. The current belief is that once the disease is triggered in a susceptible individual, there is uncontrolled inflammation in the foot. This inflammation leads to bone breaking down and is indirectly responsible for the progressive fracture and dislocation of joints in the foot.
Charcot foot symptoms, always include swelling of the foot often without a history of trauma. In the early stages there may be redness and warmth and sometimes pain. Although often diagnosed by examination and patient history x-ray is useful to confirm diagnosis. Changes to the bone that are seen on x-ray may be confused for a bone infection. A bone infection is very unlikely if the skin is intact and there is no ulcer present.
Treatment involves immobilising the foot usually with a cast or boot until the inflammation has stabilised. A Charcot episode usually results in changes to the structure of the foot often collapsing the arch of the foot resulting in a ‘rocker’ type foot. Following a Charcot episode an insole to support the foot and prevent further damage and charcot changes is required.
Contact me if you have any questions or would like further advice